The passion for climbing leads us to admire and venerate the lumbrical muscles. But in this human physical story, there’s an equally vital and fascinating supporting actor: tendons. This connective tissue, often sidelined in comparison to muscles, plays a crucial role in our ability to perform various movements, whether static or dynamic, allowing us to continuously improve our performance. What makes it so unique?
What are tendons?
Tendons, those cords that connect muscles to bones, are more than mere muscle companions. Tendons undergo a journey of adaptation and recovery slower than muscle due to their composition of ‘30% collagen, 2% elastin, and 68% water’¹. The blood supply to this connective tissue comes from four different sources: bony insertion, muscular insertion of the mesotendon or vinculum, and the paratenon. This phenomenon, where muscles grow while tendons lag behind, makes them susceptible to injuries due to repetitive and excessive use.
‘Tendinopathy’ or ‘tendonitis’
The term “tendonitis” is no longer favored because studies have shown that there is typically no inflammation present in affected tendons. Mechanobiology helps us understand how tendons adapt to stress; mechanotransduction is the process where mechanical forces trigger biochemical responses at the cellular level, stimulating cells to produce factors that aid in regeneration.
The close relationship between mechanical stress, structural changes, and biochemical alterations in the tendon matrix is crucial. These changes can lead to adaptations in the tendon’s structure, morphology, and mechanical properties.
The extracellular matrix is made up of various components found outside cells in tissues, including:
- Water
- A gel-like substance containing hyaluronic acid, proteoglycans, and glycosminoglycans
- Collagen, elastic fibers, and reticular fibers
- Fluid surrounding cells outside of them
Functions:
- Fill spaces between cells
- Allow compression and stretching of cells
- Degrade toxic waste that our body doesn’t need for purification
- Tissue regeneration
Etiology of tendinopathy
The etiology of tendinopathy, or tendon disease, is not fully understood, but three proposed conceptual models attempt to explain it: one suggests that tendon pathology arises from a primary response of tendon cells to overload, resulting in the activation and proliferation of these cells, with increases in proteoglycans leading to collagen matrix rupture and increased vascularization. Another model, the tendinous cell response model, is the most accepted, where tenocytes are responsible for maintaining balance in the extracellular matrix. There is also the inflammatory model, which hypothesizes that excessive use creates an inflammatory condition due to laceration or damage to its blood supply. Finally, the collagen rupture model, the oldest and least accepted, suggests that tendons undergo changes due to underestimation from lack of load stimulation, causing degenerative pathology through small tears, of silent and disorganized mechanical origin.
Mechanism of injury
- Constant tensile shear or compression can disrupt homeostasis, affecting the balance within the tendon.
- Repetitive tendon strain and compression are major factors in the development of tendinopathy.
Risk factors in tendinopathy
Intrinsic risk includes common medications like antibiotics, fluoroquinolones, aromatase inhibitors, and steroids. Adiposity and type 2 diabetes are established risk factors in the development of tendinopathy.
Extrinsic risk factors are environmental or external to the individual. The response to load is influenced by tendon and musculoskeletal capacity and is also affected by intrinsic factors.
For climbers, identifying peak loads or periods of biomechanical changes, such as a sudden increase in training intensity, is important.
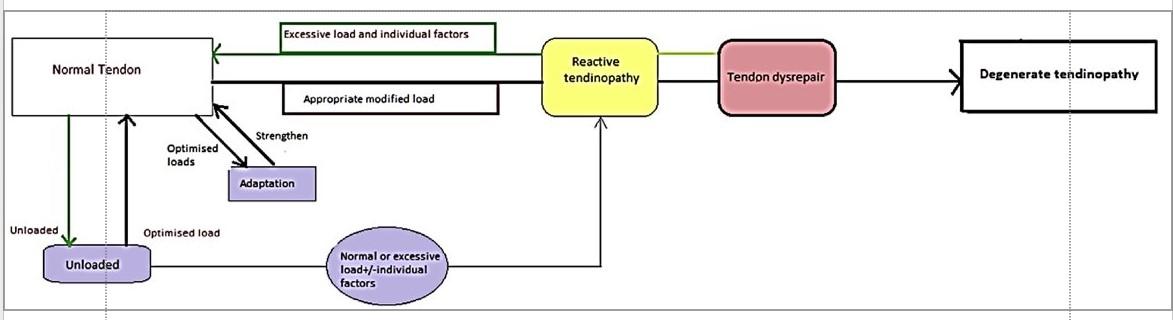
Stages of pathology
Cardoso TB, Pizzari T, Kinsella R, Hope D, Cook JL. Current trends in tendinopathy management. Best Pract Res Clin Rheumatol [Internet]. 2019;33(1):122–40.
Available at: https://www.sciencedirect.com/science/article/pii/S1521694219300233}
Three tissue states:
Reactive: Resulting from a sudden increase in physical activities the tendon isn’t accustomed to or from direct contusion.
- Described as a hyperactive cellular response to the load, with an increase in tendon cells, rounding of cells, and a significantly increased metabolic index in large proteoglycans (like aggrecan). Aggrecan is highly hydrophilic, attracting more water into the cellular matrix.
- No changes are observed in the cellular matrix in this phase.
- An altered phase of ‘healing or recovery.’
Destructured: Resulting from ‘failed recovery.’
- Generalized increase in the number of cells.
- Initiation of collagen separation and disorganization of the cellular matrix.
- The destructured tendon is asymptomatic.
- No changes in vascularization.
Degenerative: Resulting from cell changes and the appearance of neovascularization.
- Progression of collagen matrix disorganization.
- Areas of cell death due to apoptosis, trauma, or tenocyte failure.
- If tendon degeneration is extensive enough and subjected to high loads, tendon rupture could occur.
Key points
- Degenerated tendons don’t show clinical symptoms until subjected to excessive loads.
- 97% of tendon ruptures experience degenerative changes but no pain.
Are tendinopathies painful?
Tendon pains can also manifest as allodynia, a primary hyperalgesic response, and reflex in the opposite limb occasionally, but only in some tendons and not specifically in hand tendons. The continuous model highlights the strong relationship between tendon pain and mechanical load, along with tenocyte mechanosensitivity and the lack of deep tendon tissue innervation, causing nociceptor signal conduction through paracrine signaling.
Tendinopathies by evolution
- Acute: Less than two weeks.
- Subacute: Four to six weeks.
- Chronic: More than six weeks.
The acute inflammatory phase of the tendon occurs between days one to seven, with the appearance of neutrophils, monocytes, and T cells.
The proliferative phase occurs from the second day to the sixth week, with the presence of fibroblasts, macrophages, and endothelial cells.
The tendon remodeling phase occurs from the third week to twelve months with the presence of type I collagen.”
Key points
- Immobilization is contraindicated because the load on the tendon directly stimulates collagen production and alignment.
- Other studies claim that immobilizing a tendon in shortening leads to a decrease in enzymatic activity, resulting in a decrease in the effectiveness of the regenerative mechanism.
Diagnosis
- The climber can identify the site of pain with just one or two fingers.
- Pain is present when loading while climbing or hanging on the hangboard, or if there is compression of the tendon due to over-gripping.
- Tendon pain is limited when the activity is performed and disappears when the load is removed.
- The key evaluation is done 24 hours after loading that tendon.
- Classical pain assessments such as the “Visual Analog Pain Scale” are not as recommended. It is more about the pain the climber feels being tolerable and not interrupting daily function after loading. That is the best indicator.
Key points
- In the early stages, tendon pain improves with activity and worsens during rest phases.
Tendon images
- Just as there is poor correlation between abnormal tendon structure and pain, images have little diagnostic and prognostic role in tendinopathy and cannot be used as an outcome measure.

- All findings should be interpreted in relation to the clinical context
Treatment
Improving the tendon’s capacity to tolerate loads. We will start with education, control, and exercise management.
Key point
- All passive treatments do not improve tendon load tolerance.
Education
- Educating climbers has several benefits, including managing expectations for a quick solution, alleviating anxiety about imaging results, and facilitating adherence to an exercise-based rehabilitation program.
- Climbers should be aware that they may experience some discomfort during the rehabilitation program.
- Adherence is important as recovery can take many months. Discussing evidence-based treatment options will help eliminate confusion created by the plethora of available treatment options, which lack scientific basis.
Rehabilitation
- The aim is to restore tendon and muscle properties using a wide variety of exercises.
- There is evidence demonstrating the effectiveness of eccentric and slow, high-load resistance exercises (combination of eccentric and concentric). Protocols including loading appear to provide a strong stimulus to the tendon.
- An exercise-based rehabilitation program should form the core of therapy, supplemented with interventions as necessary for pain relief.
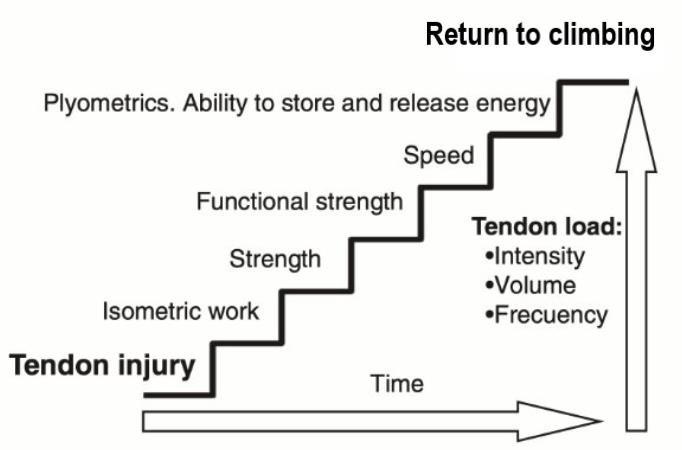
Progressive loading is the only treatment that stimulates changes in the extracellular matrix of collagen, and within the first 24 to 36 hours after loading, chemical changes in collagen degradation occur. Therefore, progressive loading or loading work needs rest periods.
Exercise-Based Rehabilitation Program for Tendinopathy in Climbers’ Hands
Isometric Exercises – Stage 1
To reduce pain, sustained isometric muscle contraction should be performed in the mid range of motion (to minimize compression loads) for 30 to 45 seconds, repeated 5 times with two minutes of rest.
Slow and Heavy Isotonic Resistance Exercises – Stage 2
The use of isometric exercises before isotonic sessions can enhance strength gains. Isotonic exercises should be performed slowly, targeting the tendon-muscle unit of the affected muscle in isolation.
For example, on the open crimp hangboard and forearm extension. These exercises should be performed on alternate days, 4 sets of 6 to 8 repetitions.
In this stage, the exercise should be pain-free for the tendon, although some muscle soreness may occur.
Key Point
Progression to the next stage is recommended when adequate strength and endurance are achieved in the affected muscle and the kinetic chain deficit improves, a process that may take up to 12 weeks.
Speed and Energy Storage Exercises – Stage 3
Based on isometric and strength and resistance exercises on alternate days. Exercises should be performed solely with body weight and involve movements of the complete kinetic chain.
Progression to the next stage depends on the tendon’s ability to tolerate faster loads.
Energy Storage and Release – Stage 4
Energy storage and release, or specific climbing exercises, may vary but must meet the criteria of Stage 3 exercises. However, exercises from Stages 1 and 2 should be maintained twice a week.
For example, rehabilitation can follow a 3-day cycle with energy storage and release exercises on day 1, performing grades below your level on day 2, and isotonic exercises on day 3.
Additional advice
Preventing recurrent tendon pain in our hands is crucial, especially for us as climbers. It requires monitoring loads, performing rehabilitation exercises during the off-season, and correcting biomechanical abnormalities by involving the healthy limb in the rehabilitation program.
About the author
Stalin Caicedo, is an experienced climber with five years of experience at Alpaca Climbing. Hailing from Ecuador, in Latin America, Stalin combines his passion for climbing with his profession as a paramedic and his academic pursuit of physiotherapy at the Catholic University of Ecuador. His dedication to healthcare and his interest in rehabilitation have led him to seek further education in physiotherapy. Outside of his professional and academic endeavors, Stalin enjoys bouldering both indoors and outdoors, making the most of his free time to explore new routes and challenges. His main focus is to promote physiotherapy tailored to climbers in his country, where information on rehabilitation advancements is limited, with the aim of improving care and treatment for local climbers.
Fore more information, check out the Instagram page @stalin_ans @alpaca_climbing
Reference
- Cook JL, Purdam C. Is compressive load a factor in the development of tendinopathy? Br J Sports Med [Internet]. 2012 [citado el 28 de noviembre de 2023];46(3):163–8. Disponible en: https://bjsm.bmj.com/content/46/3/163
- Alfredson H, Lorentzon R. Chronic Achilles Tendinosis. Sports Medicine. 2000;29(2):135–46.
- Cardoso TB, Pizzari T, Kinsella R, Hope D, Cook JL. Current trends in tendinopathy management. Best Pract Res Clin Rheumatol [Internet]. 2019;33(1):122–40. Available at: https://www.sciencedirect.com/science/article/pii/S1521694219300233}
- Couppé, C., Svensson, R. B., Silbernagel, K. G., Langberg, H., & Magnusson, S. P. (2015). Eccentric or Concentric Exercises for the Treatment of Tendinopathies? Journal Of Orthopaedic & Sports Physical Therapy, 45(11), 853-863. https://doi.org/10.2519/jospt.2015.5910
- Docking, S., Rio, E., & Cook, J. (2015). Revisiting the continuum of tendon pathology: Understanding the relationship between pain, struClimbing SIGSource